We’ve all heard whispers about fetal surgery, seen captivating stories, and perhaps known families whose journeys have taken unexpected turns. But have we paused to appreciate how extraordinary it is that contemporary medicine has ushered us into this remarkable era?
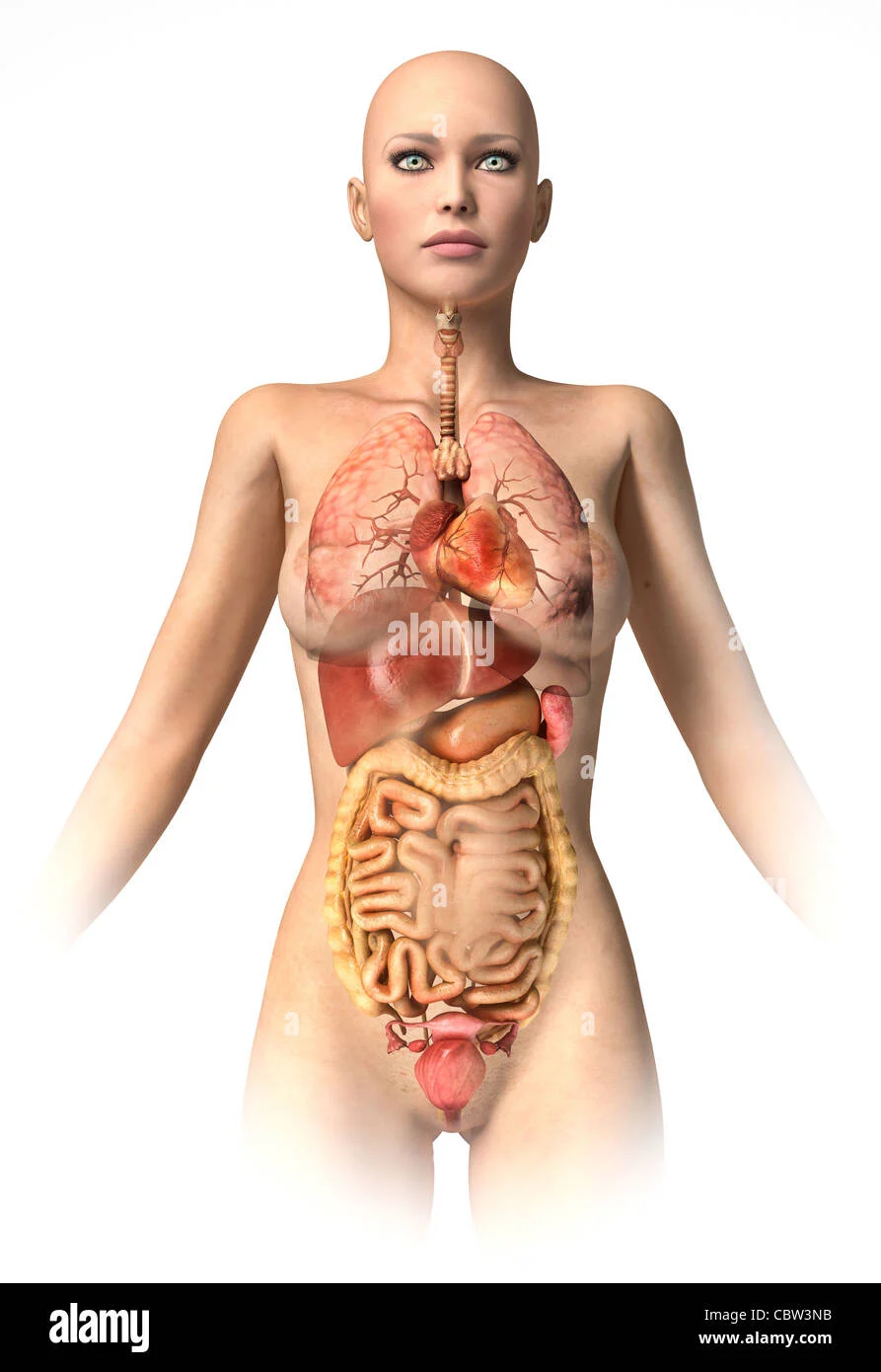
Performing surgeries on fetuses can aid countless children facing various conditions, including spina bifida, twin-twin transfusion syndrome (TTTS), and congenital diaphragmatic hernia (CDH). The fundamental concept is that addressing many birth defects while still in the womb can significantly reduce symptoms, allowing organs to develop properly before they fully function.
Take the case of a fetus with spina bifida. By closing the gap in the spine early, prior to the baby producing urine, doctors can mitigate further nerve damage in the spinal cord. For a child with CDH, if surgeons can repair the diaphragm defect promptly, it gives the baby’s lungs a chance to grow more effectively. In TTTS cases, severing the blood vessels connecting twins can help balance nutrient transfer, enabling both to thrive.
This field is not only fascinating but undeniably life-saving. However, it comes at a hefty price and can end in heartbreak. Imagine the joy of expecting a child, only to have a routine ultrasound reveal potential life-threatening conditions. It’s devastating. Yet, hope emerges in the form of surgery while the child is still in the womb—a medical marvel indeed.
Parents who pursue fetal surgery often find their lives in limbo for months. They navigate extensive paperwork, appeal insurance decisions, confront grim statistics, travel to specialized hospitals, undergo daunting surgical procedures, and prepare for the challenges of caring for a medically fragile child. They do all this knowing that, despite their efforts, their baby might not survive. Driven by the hope of giving their child a fighting chance, they embark on this journey.
Inspiring Stories of Fetal Surgery
Here are three stories that highlight how fetal surgery has impacted different families. Each faced the direst news during what should have been a joyous time, and each parent, alongside their medical team, took courageous steps to maximize their child’s chances for a fulfilling life.
In many instances, the fetuses chosen for surgery have only a slim chance of survival without intervention. For instance, Sarah Reed from San Diego learned during her 22-week ultrasound that her baby, Finn, had CDH. This condition creates a hole in the diaphragm, allowing abdominal organs to ascend into the chest cavity, which hinders lung development. With such severity, Finn’s survival odds were only 1-2%. Without surgical intervention, he had virtually no chance.
The required tracheal occlusion surgery, though not FDA-approved, might be covered by some insurance companies on a compassionate basis when survival prospects are bleak. Sarah and her husband opted for UCSF’s Fetal Treatment Center, known for pioneering fetal surgeries and specializing in CDH.
Recalling the surgery, Sarah explained that for it to succeed, Finn needed to be positioned perfectly. “Once he moved into place, they took their opportunity. They inserted a balloon the size of a grain of rice into his trachea, filling it with saline to secure it. This would occlude the trachea while I was still pregnant, creating pressure in the chest cavity to help push the organs back down, allowing his lungs to develop,” she said.
Sadly, baby Finn coughed up the balloon prematurely and lived for just 11 days, undergoing several post-birth surgeries. “I truly believe the surgery helped us,” Sarah reflected. “We never anticipated having 11 days with him. I’d do it all over again.” The total cost for Finn’s care exceeded $3 million, which was managed by the hospital and insurance.
Similarly, Emily Hart learned at her 20-week ultrasound that her son, Lucas, also had CDH. “It was devastating and surreal. One moment we were thrilled, and the next, we feared for our child’s life,” she recounted. The couple thoroughly researched options and chose to go to UCSF due to its stellar reputation.
Before the surgery, the Hart family received counseling on the potential challenges ahead. Doctors warned them that they had never had a baby with Lucas’s severity of CDH survive. “They even presented termination as an option, with 80% of families opting for it,” Emily shared.
However, she couldn’t fathom giving up. “I told my husband that we needed to explore every option for Lucas. I couldn’t bear to think about not knowing if he could have survived,” she said.
After appealing to their insurance for participation in the study, Lucas underwent the balloon placement surgery successfully. Emily was able to return home for bed rest, commuting weekly for ultrasounds. By the second week, the doctors noted remarkable lung growth, reigniting their hope.
At 31 weeks, Emily went into labor, prompting the doctors to conduct a second surgery to remove the balloon while keeping her pregnant as long as possible. Unfortunately, the procedure was complicated, and delivery became necessary. “I remember crying, overwhelmed by the reality of the situation,” she said.
“Once I woke up, I immediately asked if my baby was alive. Seeing Lucas connected to so many tubes was terrifying, but the first time I kissed him is a moment I’ll never forget,” she added. Lucas persevered through multiple surgeries and is now a vibrant 4-year-old, thanks to the fetal surgery and the dedication of his parents.
In another case, Mia Johnson discovered during her 19-week ultrasound that her daughter, Lily, had myelomeningocele, the most severe form of spina bifida. This condition can lead to paralysis due to the improper development of the backbone and spinal cord.
Mia and her husband traveled to the Children’s Hospital of Philadelphia, a leading center for fetal surgery. Research shows that performing surgery for spina bifida before birth increases the likelihood of walking, as it reduces nerve damage when done before the fetus produces urine.
Mia documented their journey, and a poignant moment came when she envisioned a day when Lily would express frustration by stomping her feet—a feat that might not have been possible without fetal surgery. After a successful procedure, Mia was on bed rest for 12 weeks before Lily’s arrival at 34 weeks.
Lily began therapy shortly after birth. “We started physical therapy within a month of coming home from the hospital. Now, at 4, she’s so functional and participates in therapy a few times a month,” Mia shared. Their insurance covered the fetal surgery, which, while FDA-approved in 2013, wasn’t guaranteed by all plans.
“We would absolutely do it all over again, knowing the risks. Lily is thriving; she walks independently with braces and displays a joyful, fulfilling life. The surgery made a significant difference,” Mia concluded.
Conclusion
Fetal surgery is a testament to modern medicine’s potential, providing hope and life-saving solutions for families facing daunting challenges.
For more information on the journey to parenthood, check out our post on at-home insemination kits here. If you’re curious about diet considerations for IVF, this resource might be helpful. Additionally, for a detailed overview of intrauterine insemination, visit Cleveland Clinic.
Summary
Fetal surgery represents a groundbreaking advancement in medicine, providing hope and life-saving interventions for families facing severe prenatal diagnoses. Through inspiring stories, we witness how these procedures can transform the lives of children and their parents, offering a fighting chance against daunting odds.