Recently, actor and writer Alex Thompson shared the joyous news of the birth of his son, Noah, after experiencing multiple late-term pregnancy losses with his partner, Jessica. In his post, Alex discussed how they had kept this pregnancy private due to their previous heartache and sought out a doctor in their Texas community who could provide support. The doctor informed them that the earlier losses were attributed to something termed an “incompetent cervix.” Alex highlighted how problematic and misogynistic this label is, prompting a laugh from the physician and a deeper appreciation from him for the doctor’s understanding.
Defining Cervical Insufficiency
Firstly, it’s commendable that Alex addressed the inherent sexism in labeling a woman’s body part as “incompetent” after enduring the trauma of pregnancy loss. It’s important to recognize that while this term has historically been associated with women, individuals who are transgender or nonbinary can also experience similar issues. The terminology of “weakened cervix” or “cervical insufficiency” is gaining traction as more appropriate alternatives that avoid placing blame solely on the woman.
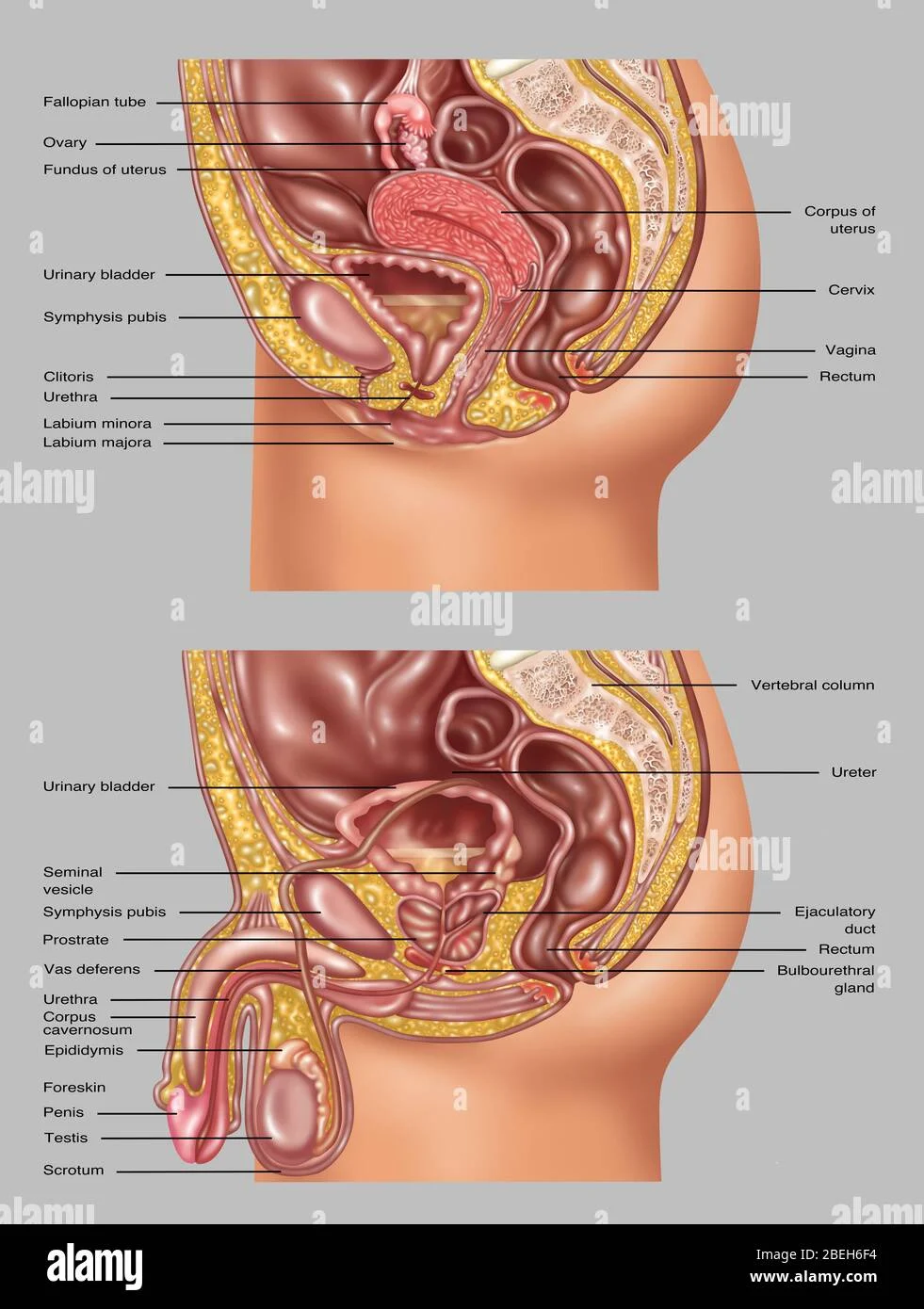
A weakened cervix refers to cervical tissue that lacks the strength to support the expanding uterus during pregnancy. The Mayo Clinic notes that this condition can lead to premature delivery or the loss of a healthy pregnancy. Normally, the cervix is firm and closed before pregnancy, but as pregnancy progresses, it softens, shortens, and dilates. A weakened cervix, however, can soften and open too early, causing significant risks.
Recognizing Symptoms and Risks
Diagnosing cervical insufficiency can be complex, often only identified after a pregnancy loss. However, there are signs to monitor, including spotting between 14 to 20 weeks, pelvic pressure, back pain, cramping, changes in vaginal discharge, or bleeding. Risk factors can include previous cervical trauma from treatments or childbirth, and studies indicate that Black women may face a higher risk of cervical insufficiency. Congenital conditions affecting the uterus or connective tissue disorders can also contribute.
Despite identifying some risk factors, a diagnosis typically doesn’t occur until after a loss, which can be heartbreaking for hopeful parents.
Options for Prevention and Treatment
Regrettably, there is no surefire way to prevent a weakened cervix. If a premature birth or late-term loss occurs, it is crucial to understand that it is not the individual’s fault. However, making healthy lifestyle choices, including regular prenatal checkups and proper nutrition, can help promote a healthy pregnancy.
If a weakened cervix is suspected, consulting with a healthcare provider is vital. They may recommend treatments to strengthen the cervix, such as medications to prevent softening or more frequent ultrasounds. A procedure known as cervical cerclage can be performed to stitch the cervix closed, providing additional support during pregnancy. This was the approach Alex and Jessica took to ensure a successful full-term pregnancy after their previous losses. Unfortunately, some practitioners may not consider this until multiple losses have occurred, which is something that needs to change to better support hopeful parents.
The pain of experiencing pregnancy loss is profound, and it’s crucial that those trying to conceive are aware of available procedures that can significantly enhance their chances of a healthy pregnancy.
For more insights on cervical insufficiency and related topics, consider visiting this blog post or check out this resource for comprehensive information on fertility and pregnancy.
Search Queries:
- What is cervical insufficiency?
- Symptoms of weakened cervix
- Cervical cerclage procedure
- Managing pregnancy risks
- Understanding pregnancy loss
In summary, the conversation surrounding cervical insufficiency is evolving, and it is essential to advocate for more compassionate language and proactive treatment options. Acknowledging the emotional toll of pregnancy loss and ensuring that individuals have access to appropriate medical care can make a significant difference in their journey toward parenthood.