In August 1994, I walked into my office one Saturday, ready to finalize a brief due in federal court on Monday. At that time, I was serving as a civil rights attorney for the justice department. Just 30 minutes into my work, an unbearable burning sensation erupted in my back, resembling acid coursing through my spine. In an instant, my muscles seized, and I found myself crumpled on the floor, overwhelmed by excruciating pain.
I was unaware then that this pain would haunt me for nearly two decades, rendering me incapable of sitting, standing, or walking without assistance. I could never have predicted that opioids would become a part of my life. Nowadays, discussions surrounding opioids are prevalent, often highlighting the tragedies of overdose and misuse. However, there’s a significant narrative that frequently goes unnoticed: opioids are among the most effective medications for managing severe pain, and for me, they were a lifeline.
With appropriate pain management that included opioids, I transitioned from being bedridden and sleepless for months to successfully negotiating major settlement agreements, presenting critical cases in federal court, and overseeing thousands of matters in U.S. attorneys’ offices nationwide. Though I had to negotiate via video calls, argue from a reclining chair, and manage cases from a makeshift platform bed, I was able to work and maintain a sense of purpose.
Sadly, today’s pain patients face challenges that I did not have to endure. In an effort to combat the serious issue of drug overdoses, many are being stripped of essential pain medications. Long-term pain sufferers who have relied on opioid analgesics are now encountering strict dosage and supply limits in numerous states, often reduced to just a few days’ worth of medication. Even in states that allow exceptions for chronic pain care, insurance companies and pharmacies often exploit these laws to deny necessary prescriptions. Patients are being involuntarily weaned off opioids, even if they have never exhibited any signs of misuse, leading to heightened suffering, diminished functionality, or even suicide.
Recently, Attorney General Mark Peterson dismissed the concerns of pain patients with a remark suggesting that “sometimes you just need a couple of aspirin and a good night’s sleep.” This statement reflects a profound misunderstanding of chronic pain, a condition that can drastically diminish one’s quality of life, comparable to late-stage cancer. In fact, nearly 50 million Americans endure severe or persistent pain, a figure that dwarfs the number of those who misuse opioids. Chronic pain is the leading cause of disability in the United States, costing our economy an astounding half a trillion dollars yearly.
It’s critical to distinguish between the legitimate use of medication for health conditions that restore function—allowing individuals to work and engage in family life—and the misuse of substances that can lead to their deterioration. Most individuals who take opioids for pain management do not abuse them; studies indicate that the risk of addiction for these patients ranges from just 0.07% to 8%. Furthermore, when opioids are prescribed responsibly—with thorough screening and ongoing care—the likelihood of addiction decreases significantly.
The majority of those who misuse prescription opioids never obtained them through medical channels; they often acquire them from home medicine cabinets, family, friends, or illicit sources. Like many others in my situation, I was initially hesitant to use opioids, exploring every other treatment option first. My chronic pain stemmed from a surgical procedure in which nerve plexuses were inadvertently damaged. I tried infusions, nerve blocks, and even another surgery, along with physical therapy, acupuncture, and biofeedback. Nothing alleviated my suffering.
Eventually, a combination of opioids and integrative therapies allowed me to keep my job and maintain a sense of community and purpose until I found a path to recovery. My experience is a seldom-told narrative of someone who responsibly used opioid analgesics for years and successfully discontinued them when my pain subsided. Unfortunately, in today’s climate, stories like mine may soon be forgotten.
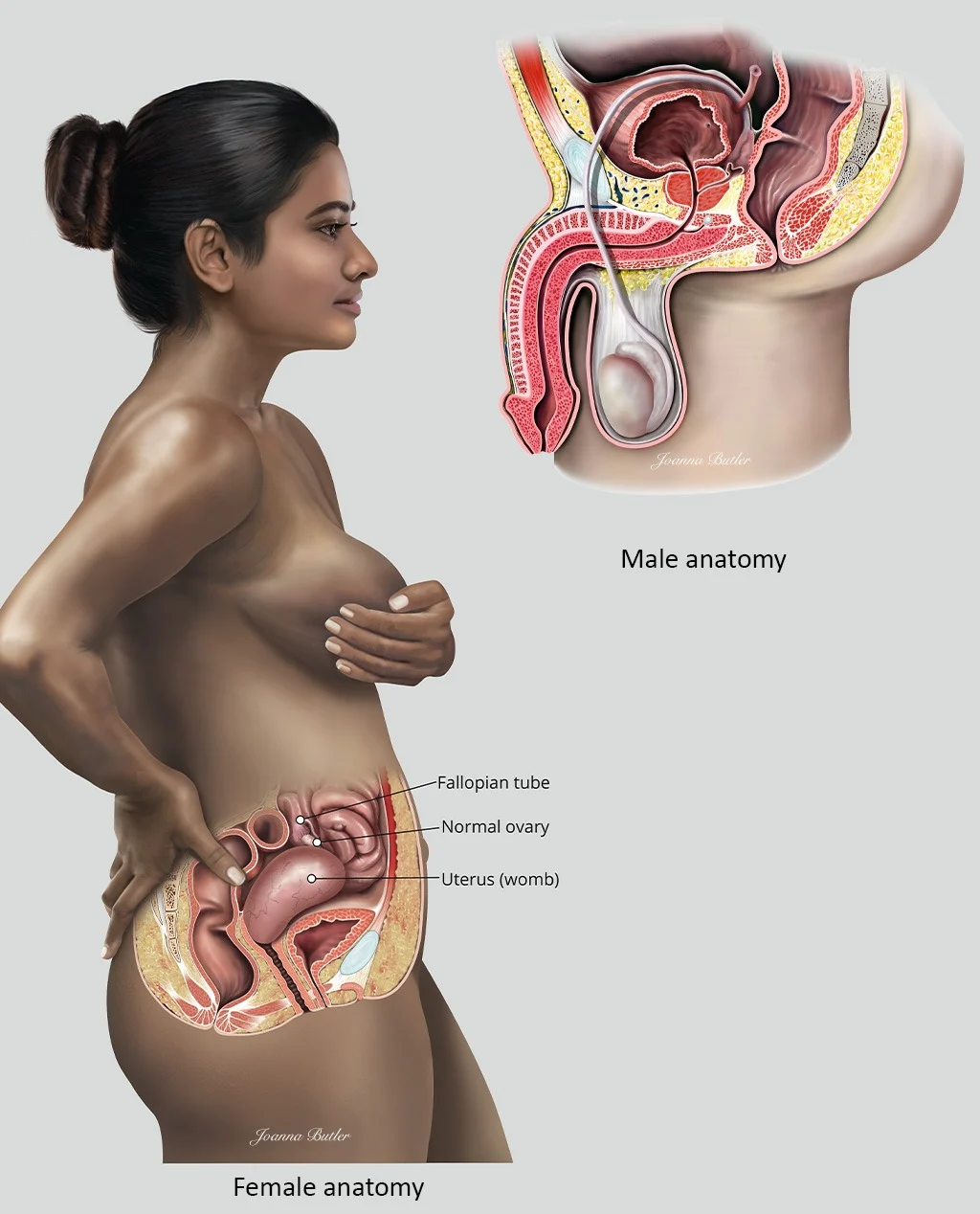
For those interested in home insemination options, check out our post on artificial insemination kits, or for more information on the process, visit intracervicalinsemination.com, where you can find authoritative resources on this topic. For those navigating pregnancy journeys, explore this excellent resource on IUI success.
Summary
The opioid crisis is often viewed through the lens of addiction and overdose, overshadowing the essential role opioids play in treating severe pain. Many pain patients face significant obstacles in accessing necessary medications, leading to increased suffering and loss of functionality. While responsible opioid use carries a low risk of addiction, current policies often neglect the needs of legitimate pain sufferers. My journey illustrates the importance of understanding the difference between responsible medication use and drug misuse.