The Science Behind Artificial Fertilization: How It Works
Artificial fertilization, also known as assisted reproductive technology (ART), has revolutionized the way people can have children. It has given hope to couples struggling with infertility, same-sex couples, and single individuals who want to become parents. But how exactly does artificial fertilization work? In this blog post, we will delve into the science behind artificial fertilization and explore the various techniques used to help people conceive.
Before we dive into the specifics, let’s first understand what artificial fertilization is. Simply put, it is the process of combining sperm and eggs outside of the body to create an embryo, which is then transferred to the uterus for implantation. This is different from natural fertilization, where sperm fertilizes an egg inside the body. Artificial fertilization involves several steps and requires the use of specialized equipment and techniques.
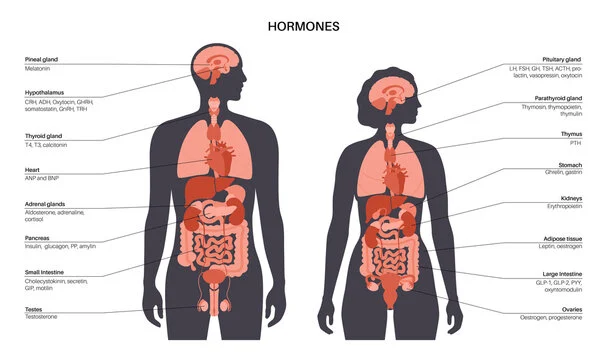
The first step in artificial fertilization is ovarian stimulation. This involves the use of fertility drugs to stimulate the ovaries to produce multiple eggs. Normally, a woman’s body releases one egg per month, but with artificial fertilization, multiple eggs are needed to increase the chances of success. Fertility drugs can be taken orally or injected, and they work by increasing the levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in the body. These hormones are responsible for stimulating the growth and maturation of eggs in the ovaries.
Once the eggs have matured, the next step is egg retrieval. This is done through a minor surgical procedure called transvaginal ultrasound aspiration. A thin needle is inserted into the vagina and guided to the ovaries to collect the mature eggs. The procedure is done under sedation, so the woman does not experience any pain. The collected eggs are then examined under a microscope to determine their quality and viability.
Meanwhile, sperm is collected from the male partner or a donor through masturbation. The sperm is then washed and prepared in the laboratory to separate the healthy and active sperm from the semen. This process is called sperm washing and is crucial in ART as it removes any impurities or dead sperm that could hinder fertilization.
The third step in artificial fertilization is fertilization itself. This can be done through two main techniques – in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). In IVF, the sperm and eggs are combined in a petri dish and left to fertilize naturally. In ICSI, a single sperm is injected into an egg to facilitate fertilization. This technique is often used when there are issues with sperm quality or quantity.
After fertilization, the embryos are monitored for a few days to ensure proper development. The healthiest and most viable embryos are then selected for transfer to the uterus. This is done through a minor procedure called embryo transfer, where a thin catheter is used to insert the embryos into the uterus. The number of embryos transferred varies depending on the woman’s age, medical history, and the quality of the embryos.
The final step in artificial fertilization is embryo implantation. This occurs a few days after the embryo transfer and is the most crucial step in the entire process. The embryo must implant into the lining of the uterus for a pregnancy to occur. If successful, the woman will have a positive pregnancy test and can continue with prenatal care to ensure a healthy pregnancy.
Now that we’ve covered the basics of how artificial fertilization works, let’s explore some common questions people have about this process.
The Science Behind Artificial Fertilization: How It Works
1. What are the success rates of artificial fertilization?
The success rates of artificial fertilization vary depending on the specific technique used, the woman’s age, and her medical history. On average, the success rate for IVF is around 30%, while ICSI has a slightly higher success rate of 40%. However, these rates can increase significantly with multiple attempts and proper medical care.
2. Can anyone undergo artificial fertilization?
Not everyone is a suitable candidate for artificial fertilization. Women with certain medical conditions such as severe endometriosis, ovarian failure, or blocked fallopian tubes may not be able to conceive through ART. In addition, the success rates decrease with age, so women over the age of 35 may have a lower chance of success.
3. Are there any risks associated with artificial fertilization?
As with any medical procedure, there are some risks associated with artificial fertilization. These include multiple pregnancies, ovarian hyperstimulation syndrome, ectopic pregnancy, and potential psychological and emotional effects. It is important to discuss these risks with a doctor before undergoing any ART procedure.
4. How much does artificial fertilization cost?
The cost of artificial fertilization varies depending on the country, clinic, and specific techniques used. On average, one cycle of artificial fertilization can cost anywhere from $8,000 to $12,000, and multiple cycles may be needed for success. It is important to research and understand the costs involved before starting the process.
5. Are there any alternatives to artificial fertilization?
Yes, there are other options for people struggling with infertility. These include intrauterine insemination (IUI), which involves placing washed sperm directly into the uterus, and surrogacy, where another woman carries the pregnancy for the intended parents. It is important to consult with a doctor to determine the best option for each individual or couple.
In conclusion, artificial fertilization has opened up a world of possibilities for people who want to become parents. It involves a series of steps that require specialized equipment and techniques, but the end result can be a successful pregnancy and a healthy baby. It is important to understand the science behind artificial fertilization and the various techniques used to make an informed decision if considering this option.