The Impact of Hormones: How Timing Affects Self-Insemination
Hormones play a crucial role in both our physical and emotional well-being. They are responsible for regulating various bodily functions and can greatly impact our moods, behaviors, and even fertility. In recent years, there has been a growing trend of individuals turning to self-insemination as a means of starting a family. While self-insemination can be a successful option, the timing of hormone levels can greatly affect its success. In this blog post, we will explore the impact of hormones on self-insemination and how timing plays a crucial role in the process.
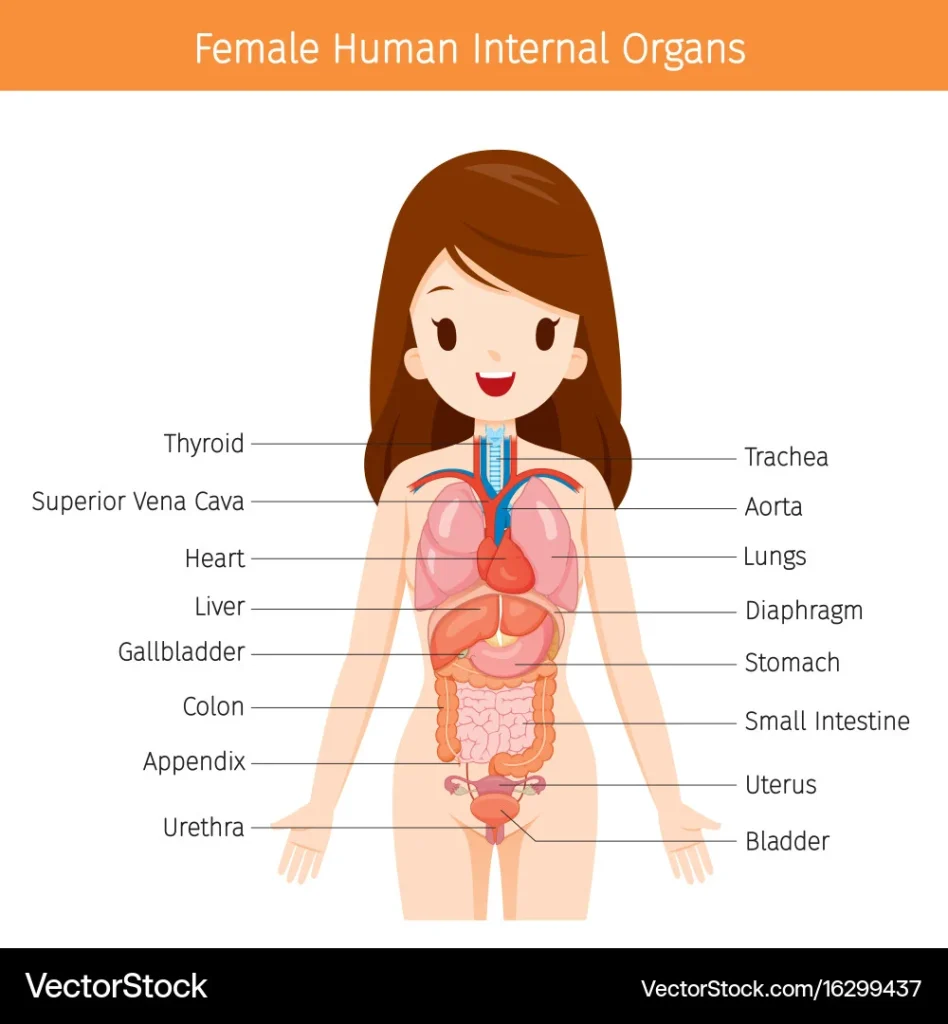
To understand how hormones affect self-insemination, we must first understand the basics of the menstrual cycle. The menstrual cycle is controlled by a complex interplay of hormones, mainly estrogen and progesterone. These hormones are responsible for the growth and release of an egg from the ovaries, as well as preparing the uterus for potential pregnancy. In a typical 28-day cycle, there are different stages, each with varying hormone levels and their own impact on self-insemination.
The first stage of the menstrual cycle is the follicular phase, which begins on the first day of menstruation. During this phase, estrogen levels start to rise, causing the lining of the uterus to thicken in preparation for a potential pregnancy. This is also the time when follicle-stimulating hormone (FSH) is released, which stimulates the development of follicles in the ovaries. These follicles contain eggs that will eventually be released during ovulation.
The next stage is ovulation, which occurs around day 14 in a typical cycle. During this time, the levels of estrogen and luteinizing hormone (LH) surge, triggering the release of an egg from the ovary. This is the most crucial time for self-insemination, as it is the only time when an egg is available for fertilization. However, the window for fertilization is relatively short, with the egg only being viable for 12-24 hours after ovulation.
After ovulation, the luteal phase begins. During this phase, progesterone levels increase, further thickening the uterine lining and preparing it for a potential pregnancy. If fertilization does not occur, hormone levels will eventually drop, leading to the shedding of the uterine lining and the start of a new cycle.
Now that we have a basic understanding of the menstrual cycle and hormone levels, let’s dive into the impact of timing on self-insemination. As mentioned earlier, ovulation is the most crucial time for self-insemination, as it is the only time when an egg is available for fertilization. Therefore, timing is key when it comes to self-insemination success. The key to successful self-insemination is to predict when ovulation is most likely to occur and time the process accordingly.
The Impact of Hormones: How Timing Affects Self-Insemination
One method of predicting ovulation is by tracking basal body temperature (BBT). BBT is the lowest body temperature recorded in a 24-hour period, and it rises slightly after ovulation due to an increase in progesterone. By tracking BBT, individuals can pinpoint when ovulation occurs and time self-insemination accordingly.
Another method is by using ovulation predictor kits (OPKs), which detect the presence of LH in urine. As mentioned earlier, LH levels surge just before ovulation, making it a reliable indicator of when ovulation is about to occur. OPKs can be used in conjunction with BBT tracking to confirm ovulation and increase the chances of successful self-insemination.
Aside from timing, hormones can also impact the quality of cervical mucus, which plays a crucial role in self-insemination. Cervical mucus is a fluid produced by the cervix that helps sperm travel to the egg. It changes in consistency and volume throughout the menstrual cycle, becoming thinner and more slippery around ovulation to allow sperm to pass through more easily. However, hormonal imbalances can affect the quality of cervical mucus, making it difficult for sperm to reach the egg.
In addition to these factors, hormones can also impact the overall fertility of individuals. Conditions such as polycystic ovary syndrome (PCOS) and thyroid disorders can cause hormonal imbalances, making it more challenging to conceive through self-insemination. It is crucial to consult a healthcare provider if you suspect any underlying hormonal issues that may be affecting your fertility.
In conclusion, hormones play a significant role in self-insemination, and timing is crucial for its success. By understanding the impact of hormones on the menstrual cycle and using methods such as BBT tracking and OPKs, individuals can increase their chances of successful self-insemination. It is also essential to address any underlying hormonal imbalances that may affect fertility and seek medical advice if needed.
5 Probable Search Queries:
1. “How do hormones affect self-insemination?”
2. “Timing and self-insemination: why it matters”
3. “The role of hormones in fertility and self-insemination”
4. “Tips for successful self-insemination: understanding hormone levels”
5. “Hormonal imbalances and self-insemination: what you need to know”