I was several months into my third pregnancy when I first felt it—an intense discomfort that made its presence known after long periods on my feet or during the simple act of getting in and out of bed. It felt as if I had taken a direct hit in my pelvic region—no kidding! Initially, I suspected I had bruised my pubic bone, but I couldn’t recall any incident that might have caused it.
As a seasoned mom, I understood that aches and pains could be a routine part of the pregnancy journey. My previous pregnancy had introduced me to severe round ligament pain that felt like a knife in my side, but that was fleeting. This new discomfort ranged from a persistent dull ache to sharp pangs that seemed endless.
It hurt to stand too long. Walking was a challenge. Getting in and out of the car? Painful. Even stretching my legs more than shoulder-width apart sent shockwaves of discomfort through me. Essentially, moving felt like a trial.
I consulted two different doctors about this troubling pain, both of whom offered similar reassurances: “It’s likely just the baby putting pressure on your pelvis. Feeling pressure down there is perfectly normal.” I tried to explain that as a third-time mom, I recognized the feeling of pelvic pressure and this was something entirely different—this was a sharp pain, localized right at my pubic bone. “Sure, many aches and pains are common,” they replied, seemingly dismissing my concerns.
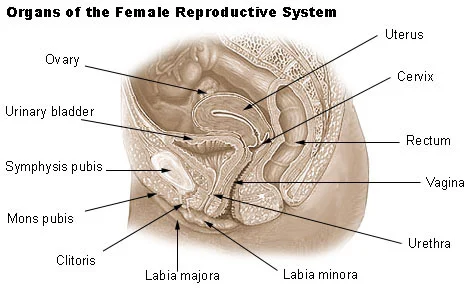
I wasn’t a medical professional, but like many people today, I turned to the internet for answers. A search for “pain in the crotch during pregnancy” led me to the term I had been seeking: symphysis pubis dysfunction, or SPD. It sounds more like a disease than a pregnancy issue, but it occurs when the relaxin hormones cause excessive loosening of the pelvic bones. This can lead to separation of the joint connecting the pubic bones, resulting in a range of painful sensations in the pelvic area, often labeled as pelvic girdle pain.
However, “pelvic girdle pain” sounds relatively benign and doesn’t do justice to the intensity of what I felt. Unless I was cautious about how much I walked or stood, I endured hours of excruciating discomfort. At six months pregnant, grocery shopping became an impossible task; I had to rely on one of those motorized carts. I usually enjoyed being active during my pregnancies, but now I could barely manage five minutes of walking without facing repercussions for the rest of the day.
Even simple actions like rolling over in bed or spreading my legs involved sharp, stabbing pains (yes, even during intimacy, although some positions were tolerable). After doing a deep dive into my online research, I returned to my doctor and shared my findings. “Hmm, that could be it,” he acknowledged. (Why didn’t you mention that before?) He suggested I try a support belt.
I bought one, and while it offered some relief, I found that chiropractic adjustments and acupuncture were more beneficial, though nothing provided a complete cure. There were stories of women who found significant relief through chiropractic care, but my experience was more stubborn. I even read that, in rare cases, SPD could persist after childbirth. What a nightmare!
Fortunately, my SPD symptoms vanished almost immediately after giving birth, which was a huge relief. I wouldn’t wish that experience on anyone.
My struggles with SPD are not entirely uncommon. Statistics on SPD vary widely: some sources claim 1 in 300 pregnant women experience it, while others suggest it could be as high as 1 in 5. Two of my friends dealt with it during their pregnancies, and countless stories online echoed my experience. Many women reported that their doctors initially dismissed their symptoms as typical pregnancy discomfort.
Trust me, there’s nothing “normal” about feeling as if a bowling ball was dropped on your pubic bone. The pain can range from moderate to excruciating—I definitely fell into the latter category. If you ever felt a grinding sensation or sharp pain in your pubic area while pregnant, you might have experienced undiagnosed SPD.
If you’re currently pregnant and dealing with soreness in your pubic bone, don’t hesitate to speak with your doctor about it. It’s surprising how little awareness surrounds such a common pregnancy issue, likely because it’s not something people openly discuss. “Hi there, sorry, but my pubic area is in serious pain today.” And then explaining I have symphysis pubis dysfunction? No thanks.
If you’ve experienced SPD or are coping with it now, I truly sympathize with you. It can be incredibly challenging, but just know you’re not alone in this journey. Solidarity, SPD sisters!
For more insights on pregnancy-related issues, check out this helpful article from Intracervical Insemination, and if you’re interested in home insemination, you can learn more about it by visiting this guide.
In summary, if you’re dealing with SPD, it’s crucial to seek support and information. You’re not alone, and understanding your body can lead to better management of this often-overlooked condition.