I’ve undergone eight surgeries in my life, all without significant complications. While it’s normal to feel anxious before a procedure, no one prepares for unexpected post-operative issues, especially after what should be a routine surgery. When I had my recent partial hysterectomy, I certainly didn’t expect to find myself back in the ER that same night.
Waking up from the surgery was agonizing. I’ve experienced three c-sections, which I thought were painful, but the discomfort I felt in recovery after my hysterectomy was on an entirely different level. At one point, I told my nurse it felt like my bladder was about to burst. She seemed irritated, repeatedly reminding me that I had already attempted to use the bathroom several times. “You don’t have enough urine to go,” she snapped. I took her at her word.
Throughout my time in post-op, my pain was relentless. I couldn’t find a comfortable position and felt an overwhelming need to relieve myself. I didn’t feel ready to leave, but soon I was being discharged, too uncomfortable to argue. I thought being in my own bed would help ease the pain, so I left without protest.
Later that night, despite taking the maximum dose of pain medication, I was even more miserable and made the decision to return to the ER. That’s when I discovered my bladder was extremely full—really full.
It turned out I had Acute Post-Operative Urinary Retention (POUR). I never thought I would beg for a catheter, but there I was, pleading with my compassionate nurse. The relief was immediate; imagine having to hold it for 13 hours after being given fluids and finally being able to let go. It was a tremendous relief.
Finally, I could lie comfortably without that awful pressure. My nurse even remarked, “I bet you’re feeling better!” as she watched my catheter bag fill up. I ended up needing a catheter for a week and a straight catheter for three days afterward. I gained a new respect for those who rely on catheters all the time.
Unfortunately, I ended up with a urinary tract infection (UTI) and a yeast infection, which are common side effects of catheter use, but still unpleasant. The catheter was uncomfortable, and I constantly worried about kinks in the tubing and where to hang the bag while I slept.
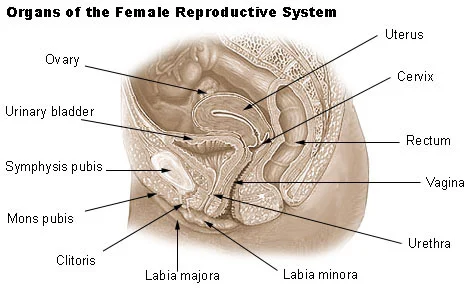
During this time, I relied heavily on support from my husband. I never envisioned squatting over the toilet with him while I held a straight catheter and a mirror while he shone a flashlight on my urethra. It was humiliating and not a topic I felt comfortable discussing outside of my inner circle.
This experience was indeed humbling. It wasn’t until I went through it that I realized how prevalent this complication can be. According to a medical journal on NCBI, post-operative urinary retention can affect between 5% to 70% of patients, with higher rates in those undergoing spinal, epidural, or general anesthesia. It’s particularly common after pelvic surgeries, especially gynecological ones, and can also occur after orthopedic surgeries where nerves affecting urination may be impacted.
Interestingly, while I was acutely aware of my urinary retention, one study showed that 60% of outpatient surgical patients experienced no symptoms of retention despite having a full bladder. This highlights the need for greater awareness surrounding this common post-operative issue.
Symptoms to Watch For
After any outpatient procedure, patients should inform their healthcare provider if they experience acute retention symptoms, such as:
- Inability to urinate or no urge to urinate eight hours post-surgery
- A painful urge to urinate
- Swelling or pain in the lower abdomen
Acute urinary retention is a medical emergency and can sometimes present with subtle symptoms. Keeping a record of your urination habits during recovery is advisable. In contrast, chronic urinary retention may manifest with less noticeable signs, such as difficulty starting to urinate, a feeling of incomplete bladder emptying, or an inconsistent stream.
Monitoring your urinary output and frequency is crucial after surgery. Even if you aren’t in pain, it’s wise to contact your doctor if you suspect urinary retention. Ignoring these symptoms can lead to long-term damage to your bladder or urinary tract.
My post-operative urinary retention likely stemmed from the type of surgery I had. While I wouldn’t say I was fortunate to experience such pain, it may have been a blessing in disguise that led me to seek help promptly.
For those interested in more information about home insemination, check out some of our other blog posts, like this one. And if you’re looking for an authoritative source on related topics, visit Intracervical Insemination, which provides valuable insights. Additionally, UCSF’s resource on IVF is an excellent guide for pregnancy and home insemination.