After welcoming my first baby into the world, the last thing I was thinking about was intimacy with my partner. Between sleepless nights, constant nursing, and a challenging recovery, any desire for sex vanished. While I longed for closeness, the thought of any penetration was daunting.
When my doctor finally gave me the green light to resume sexual activity, I was unprepared for the experience that awaited me. It was excruciating, and it took weeks before I felt fully healed. This period strained my relationship, as we had once enjoyed a fulfilling sex life. I felt betrayed by my body, while my partner was distressed by my discomfort.
Eventually, my physical issues improved, but the feelings of embarrassment and isolation lingered. I had never heard my friends discuss pain during intercourse, leading me to believe I was the only one suffering.
However, I soon discovered that I was not alone. Many women experience a condition known as vaginismus, characterized by involuntary vaginal tightening that results in discomfort, burning, or pain during penetration. Some women may struggle even with the insertion of tampons. Estimates suggest that approximately 2 in every 1,000 women deal with vaginismus, although accurate statistics are difficult to obtain due to the stigma surrounding the condition. Many women are misdiagnosed, and healthcare providers often overlook the specific challenges related to vaginal penetration.
It’s important to understand that if you are experiencing vaginismus, your struggles are valid and not merely psychological. Past trauma or abuse can sometimes be linked to the condition, although this is not universal. Researchers often connect vaginismus to anxiety and fear related to sexual activity. It’s no wonder that a woman would feel anxious about a painful experience.
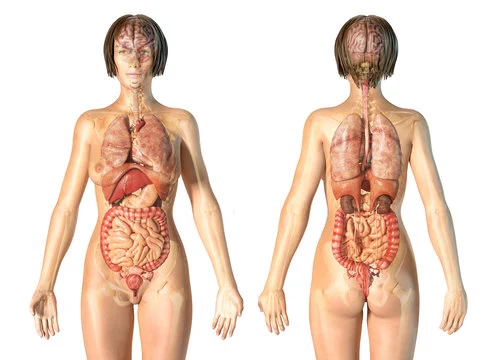
Women describe the sensation of trying to have sex as akin to “bumping into a wall,” which is tied to the involuntary contraction of the pelvic floor muscles, particularly the pubococcygeus (PC) group. These muscles can spasm so tightly that even a tampon cannot be comfortably inserted.
To be clear: Vaginismus is not just “all in your head.” It is a genuine condition that requires attention.
While there is currently no known cure for vaginismus, there are ways to manage and reduce the symptoms of painful intercourse. Seeking a proper diagnosis from a gynecologist or healthcare provider is crucial, and it’s essential to communicate openly about your experiences—many others share your struggle.
If vaginismus is confirmed, treatments often include exercises aimed at gaining control over the vaginal muscles. Kegel exercises can be particularly helpful in relaxing these muscles. Over time, these exercises can desensitize the pelvic floor, making penetration more manageable. A healthcare provider can guide you through the process, teaching you how to effectively engage your pelvic muscles—those same muscles you use to stop urination. Over time, you can work toward progressively more challenging steps, such as gently inserting a finger, all aimed at retraining your body to dissociate penetration from pain.
Importantly, vaginismus can significantly impact relationships, leading to unconsummated marriages or a lack of intimacy. If you find yourself in this situation, know that help is available. Seeking resources and treatment is key to reclaiming your sexual health and enjoying intimacy with your partner.
For more information on fertility and home insemination, check out this useful resource on pregnancy and infertility. Additionally, for insights from medical professionals, Dr. Emily Johnson’s discussion on IVF advancements offers valuable perspectives.
Summary:
Experiencing painful sex is a common issue that many women face, often linked to a condition known as vaginismus. This involuntary tightening of the vaginal muscles leads to discomfort during penetration and can stem from various factors, including anxiety or past trauma. While there is no cure, women can work with healthcare providers to explore treatment options, including pelvic floor exercises like Kegels to help manage symptoms. Support and resources are available to help individuals navigate this sensitive issue and improve intimacy with their partners.