Ovulation is a crucial part of the menstrual cycle for women as it plays a significant role in fertility and pregnancy. During ovulation, an egg is released from the ovary and travels through the fallopian tube, where it can potentially be fertilized by sperm. However, this process can be affected by sexually transmitted infections (STIs), which can have severe consequences for fertility and pregnancy.
STIs are infections that are spread through sexual contact, including vaginal, anal, and oral sex. Some of the most common STIs include chlamydia, gonorrhea, syphilis, human papillomavirus (HPV), and herpes. These infections can have a significant impact on a woman’s reproductive health, including her ability to conceive and carry a healthy pregnancy.
In this blog post, we will explore the relationship between ovulation, STIs, and their impact on fertility and pregnancy. We will also discuss the importance of STI prevention and treatment for women who are trying to conceive or are pregnant.
How STIs Affect Ovulation
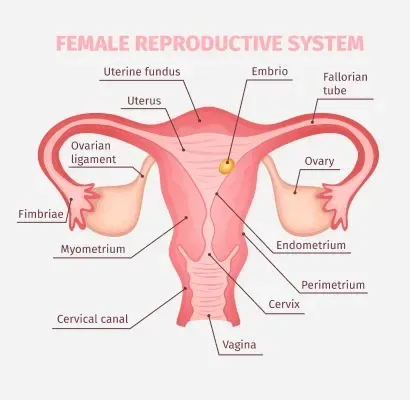
STIs can affect ovulation in several ways. Firstly, they can cause inflammation and damage to the reproductive organs, such as the cervix, fallopian tubes, and ovaries. This can lead to scarring and blockages, making it difficult for the egg to travel through the fallopian tube and be fertilized by sperm.
Moreover, some STIs, such as chlamydia and gonorrhea, can cause pelvic inflammatory disease (PID), a serious infection that affects the reproductive organs. PID can cause permanent damage to the fallopian tubes, which can lead to infertility and increase the risk of ectopic pregnancy (a pregnancy that occurs outside the uterus).
STIs can also affect the cervical mucus, which plays a crucial role in the fertilization process. During ovulation, the cervical mucus becomes thin and slippery, allowing sperm to swim through it easily. However, STIs can cause changes in the cervical mucus, making it thicker and less hospitable to sperm, making it difficult for them to reach the egg.
The Impact of STIs on Fertility
The presence of STIs can significantly decrease a woman’s fertility. According to the Centers for Disease Control and Prevention (CDC), untreated chlamydia and gonorrhea can lead to infertility in up to 30% of women. Furthermore, women with untreated chlamydia or gonorrhea are seven times more likely to have difficulty getting pregnant than those without these infections.
Ovulation and Sexually Transmitted Infections: The Impact on Fertility and Pregnancy
In addition, STIs can also increase the risk of miscarriage and stillbirth. For example, untreated chlamydia can lead to scarring of the fallopian tubes, which can increase the risk of an ectopic pregnancy. If left untreated, ectopic pregnancies can be life-threatening for the mother and often result in the loss of the pregnancy.
STIs and Pregnancy
Pregnant women with STIs also face a higher risk of complications. Some STIs, such as syphilis and HIV, can be passed from the mother to the baby during pregnancy or delivery. This is known as vertical transmission and can have serious consequences for the baby’s health, including birth defects, developmental delays, and even death.
Moreover, STIs can also increase the risk of preterm labor and low birth weight. These conditions can have long-term effects on the baby’s health and development. It is essential for pregnant women to get tested for STIs regularly and receive treatment if needed to protect their health and the health of their baby.
STI Prevention and Treatment
The best way to prevent the negative impact of STIs on fertility and pregnancy is to practice safe sex. This includes using condoms and getting tested for STIs regularly, especially if you have multiple sexual partners.
If you do get diagnosed with an STI, it is essential to get treatment as soon as possible. Many STIs can be easily treated with antibiotics, but it is crucial to complete the full course of treatment to ensure that the infection is completely cleared.
It is also essential for your partner to get tested and treated to prevent re-infection and potential complications. If you are trying to conceive, it is recommended to wait until both partners have completed treatment and have tested negative for the infection before having unprotected sex.
Summary:
Ovulation is a critical part of the menstrual cycle for women, but it can be affected by sexually transmitted infections (STIs). STIs can cause inflammation and damage to the reproductive organs, leading to scarring and blockages that can affect a woman’s fertility. These infections can also increase the risk of complications during pregnancy, including miscarriage and stillbirth. To prevent the negative impact of STIs on fertility and pregnancy, it is essential to practice safe sex and get tested regularly. If diagnosed with an STI, prompt treatment is crucial for both partners to prevent further complications.