Menstrual pain is often dismissed as a minor inconvenience, but for many women, it is a debilitating experience that goes far beyond mere cramping. The agony can manifest throughout the body, including symptoms like gastrointestinal distress—such as diarrhea and nausea—alongside backaches and severe cramps that may leave one incapacitated.
Dr. Elizabeth Hale, an expert in reproductive health at the University of Cambridge, has voiced a resonating truth: menstrual discomfort can be “almost as debilitating as a heart attack.” This statement has been met with a sigh of relief from countless women who feel validated in their suffering. The reality is that menstrual pain is not merely a figment of our imagination; it is a genuine medical condition that deserves attention and treatment.
Many healthcare professionals have long held the belief that over-the-counter medications like ibuprofen are sufficient for managing this pain, but for those who endure excruciating cramps, such remedies can feel inadequate. While not every woman experiences incapacitating pain, it is common to encounter at least one cycle that feels overwhelming, reminiscent of being physically attacked from within.
Dysmenorrhea: Understanding Painful Periods
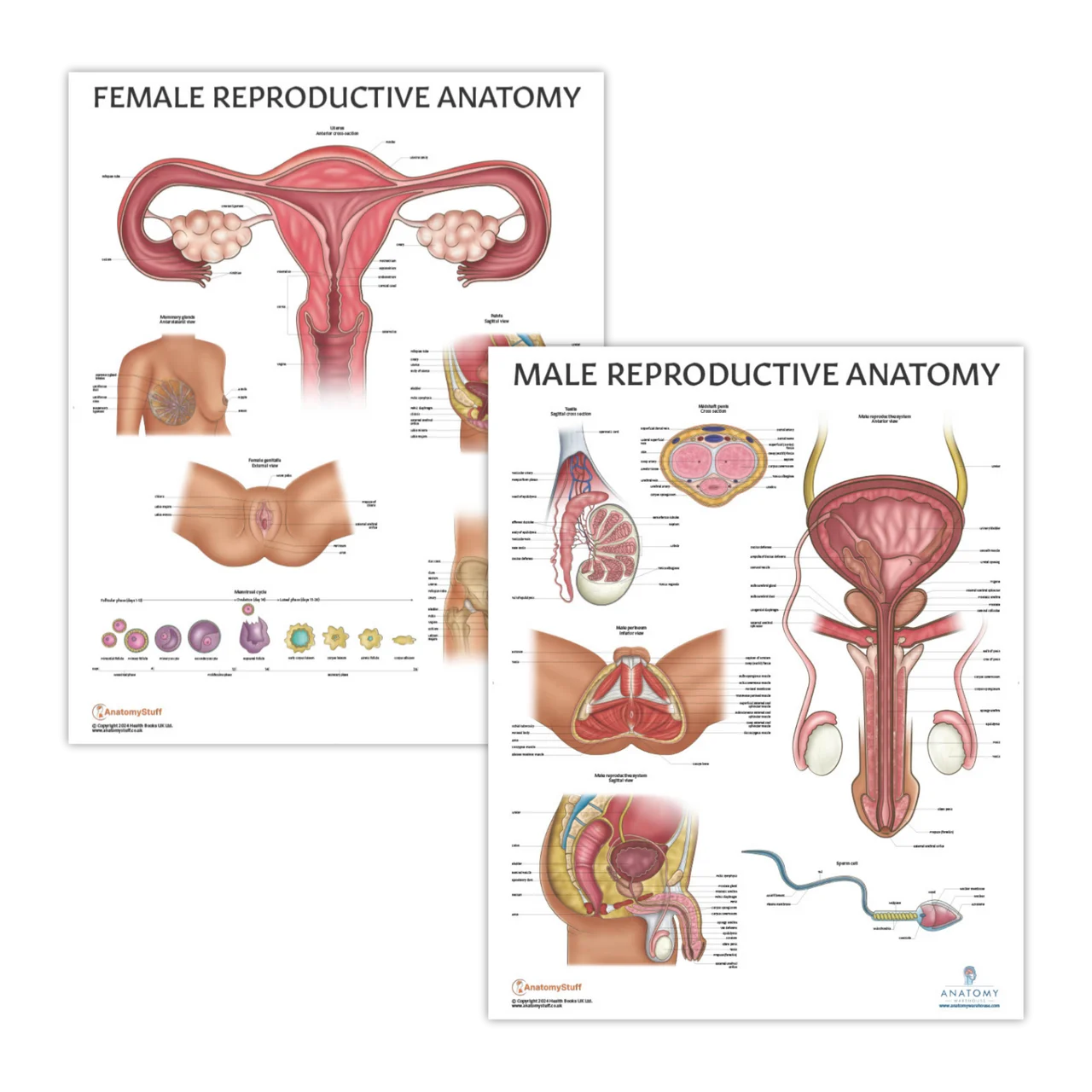
Painful periods, medically termed “dysmenorrhea,” affect a significant portion of the female population—up to 20% of women report severe symptoms that disrupt their daily lives. Younger women are more frequently affected, and many report that their symptoms lessen with age. Dysmenorrhea is classified into two types: primary dysmenorrhea, which refers to standard severe menstrual pain, and secondary dysmenorrhea, which is linked to underlying conditions like endometriosis or ovarian cysts.
Endometriosis, characterized by the presence of uterine tissue outside the uterus, is notorious for causing extreme menstrual pain. Alarmingly, this condition impacts around 10% of women who ovulate, yet it often goes undiagnosed for years—sometimes as long as a decade—delaying crucial treatment.
The Need for Change in Medical Response
This highlights the urgent need for the medical community to take female patients’ pain seriously. Dr. Hale emphasized that if men experienced this kind of monthly torture, the medical response would undoubtedly be swifter and more comprehensive. “Men don’t understand it, and women’s pain has not been prioritized,” she noted.
Dr. Samuel Wright from the National Institute of Women’s Health has echoed these sentiments, stressing the necessity for broader treatment options for painful periods and urging more research into the subject. He also encourages women to share their experiences openly, despite the stigma surrounding these discussions. “We need to normalize conversations about menstrual pain on platforms like national television,” he asserts.
Finding Support and Resources
For those suffering, it is imperative to find healthcare providers who listen and respond with empathy. The phrase “just take an Advil” is insufficient when one is experiencing pain that feels like a fire in the uterus. Pain management must be taken seriously and addressed comprehensively.
In the realm of home health, understanding one’s body is crucial. You may find useful information on topics like home insemination and pregnancy through excellent resources such as IVF Babble. For those considering family planning, you can explore the BabyMaker at Home Insemination Kit for more information on self-insemination techniques. Additionally, for those curious about prime day deals related to health products, visit this link for insights.
Conclusion
In summary, menstrual pain is a significant health issue that warrants serious attention and treatment. Women should not have to suffer in silence, and open dialogue about these experiences is vital for driving change in healthcare.