When my first child was born, I encountered the common “baby blues.” I distinctly remember cradling him on the couch just days after his birth, overwhelmed by waves of tears for no clear reason. Both the parenting books and my medical team assured me that what I was feeling was typical and that it would pass without concern.
As the months rolled on, moments of profound sadness and anxiety would creep in, often interspersed with panic. I’d find myself waking in the night, heart pounding, checking to ensure my baby was still breathing. At times, even everyday situations, like driving home or waiting for my son to fall asleep, would trigger intense feelings of dread.
During these episodes, the emotions felt so intense that they seemed unbearable. Yet, these feelings would eventually subside, and overall, I felt content as a new mother, leading me to believe there was no underlying issue.
Fast forward to the toddler years, and my mental health took a dramatic turn. I found myself grappling with severe depression and panic disorder, unlike anything I had previously experienced. Several factors likely contributed to this: a traumatic incident when my son fainted and required hospitalization (thankfully, he was okay), an unexpected miscarriage that I hadn’t realized was happening, and ongoing conflicts with family members. Plus, let’s be honest—toddler tantrums can be far more exhausting than newborn fussiness.
It took me years to recognize that I might have been dealing with an untreated case of postpartum depression (PPD) or anxiety that had manifested later. This realization aligns with a growing understanding in the mental health community about the phenomenon known as “toddler blues” or late-onset PPD, which is gaining recognition.
Most people are unaware that PPD isn’t limited to the early months after childbirth. According to the American College of Obstetricians and Gynecologists (ACOG), postpartum depression can occur up to a year after giving birth. However, Karen Maxfield, a mental health expert, suggests this timeframe is too restrictive. She highlights that symptoms of depression and anxiety can emerge at various stages beyond the initial postpartum period.
It’s important to note that while we can’t attribute later symptoms directly to PPD if our children are significantly older, the notion that the impacts of PPD can extend well beyond one year is gaining traction. Maxfield points out that the spectrum of postpartum distress may last longer than previously thought, indicating that many women continue to struggle with mental health issues long after their initial postpartum phase.
In my case, it felt as though my PPD had been building over the years, culminating in a significant crisis during my son’s toddler stage. Kate Lark, a licensed clinical social worker specializing in maternal mental health, refers to this as “continued postpartum distress.” She often sees mothers who, even years after giving birth, are facing challenges rooted in their pregnancy or postpartum experiences.
The key takeaway is that women deserve better support and care during and after pregnancy. There needs to be a reduction in the stigma surrounding postpartum mood disorders, as many women hesitate to seek help, prioritizing the needs of others over their own well-being. Moreover, access to mental health services is crucial; it shouldn’t be a privilege but rather a necessity for mothers striving to care for themselves and their families.
Had I sought help for my initial symptoms, I believe my later struggles could have been mitigated. Those months of “toddler blues” were excruciating, but after returning to therapy, I finally found the support I needed. I wish I had known earlier that what I was experiencing had a name, that it was valid, and that I didn’t have to endure it silently.
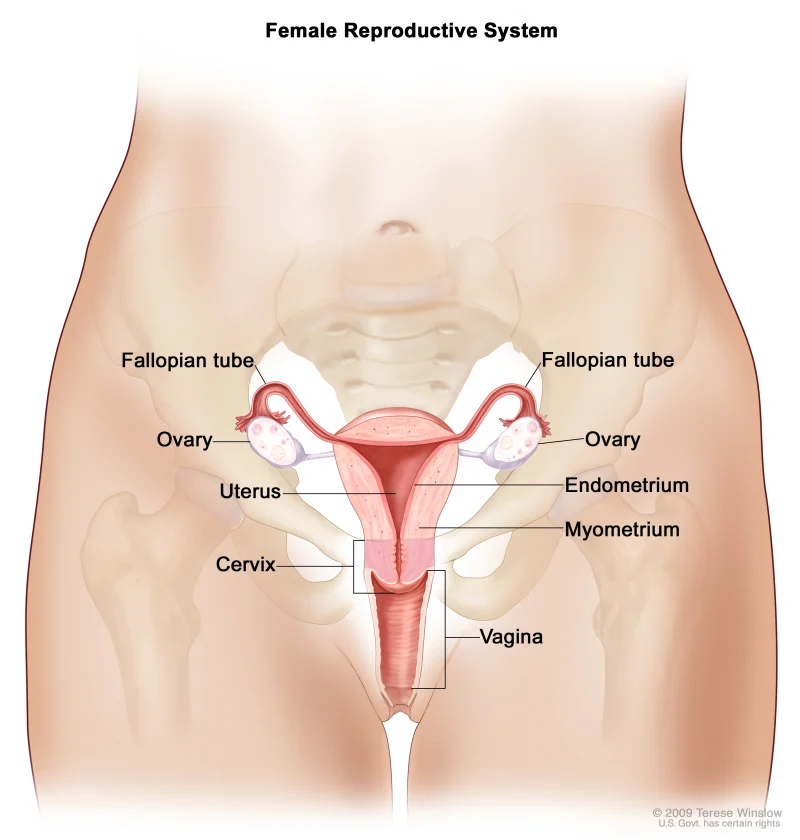
For those looking for additional resources on mental health during and after pregnancy, check out MedlinePlus for comprehensive information on pregnancy and the journey of home insemination. Also, for insights into recognizing and understanding infant birthmarks, visit the experts at Intracervical Insemination.
In summary, acknowledging and addressing postpartum mood disorders is crucial for the well-being of mothers. The journey through motherhood can be overwhelming, but with the right support, no one has to face it alone.