In Vitro Fertilization: A Breakthrough in Assisted Reproductive Technology
In vitro fertilization (IVF) is a revolutionary assisted reproductive technology that has helped millions of couples and individuals around the world to overcome infertility and start a family. It involves the fertilization of an egg outside of the body, in a laboratory setting, and then transferring the resulting embryo back into the uterus. Since its introduction in the late 1970s, IVF has continuously evolved and improved, making it a highly successful and widely used method for achieving pregnancy. In this blog post, we will explore the history, process, success rates, and ethical concerns surrounding IVF, as well as its impact on society and the future of reproductive technology.
History of IVF
The first successful IVF procedure was performed in 1978 by British scientists, Dr. Robert Edwards and Dr. Patrick Steptoe, who helped a woman with blocked fallopian tubes to conceive and give birth to a healthy baby girl, named Louise Brown. This breakthrough in medical science gave hope to millions of couples struggling with infertility, and since then, IVF has become the most widely used assisted reproductive technology.
Over the years, advancements in IVF technology have increased its success rates and made it more accessible to a larger population. In the 1980s, the use of fertility drugs to stimulate the ovaries and produce multiple eggs for retrieval was introduced, leading to a significant increase in pregnancy rates. In the 1990s, the development of a technique called intracytoplasmic sperm injection (ICSI), where a single sperm is injected directly into an egg, provided an effective solution for male factor infertility. In recent years, the use of preimplantation genetic testing (PGT) has further improved the success rates of IVF, by allowing the selection of genetically healthy embryos for transfer.
The IVF Process
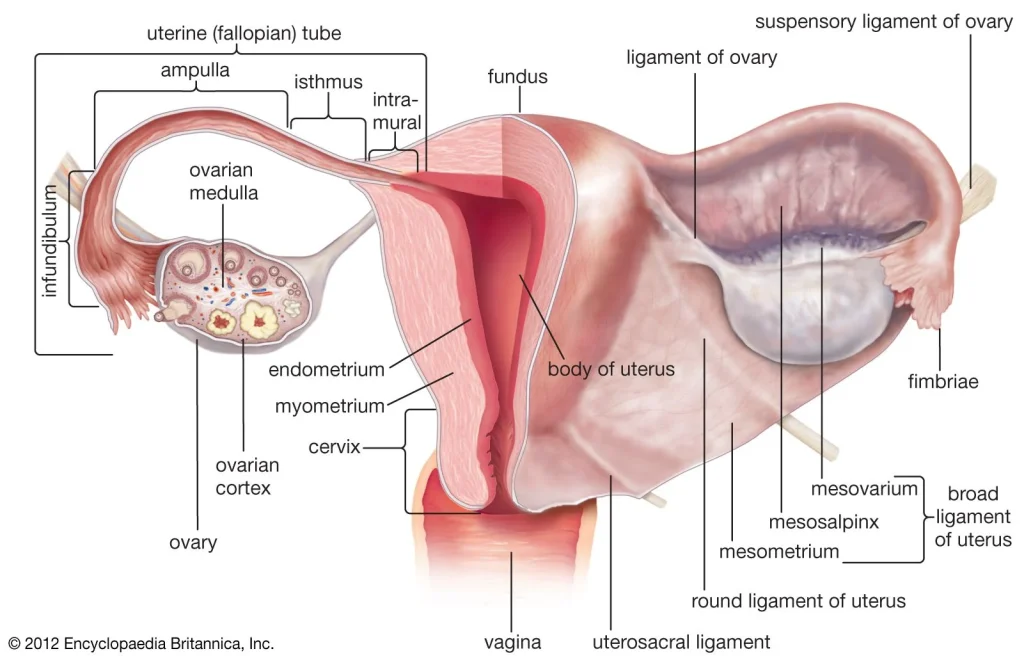
The IVF process consists of several steps, starting with ovarian stimulation, where fertility drugs are used to stimulate the ovaries to produce multiple eggs. This is followed by egg retrieval, a minor surgical procedure where the eggs are collected using a thin needle, guided by ultrasound. The eggs are then fertilized in the laboratory, either through traditional IVF, where the eggs and sperm are placed together in a culture dish, or through ICSI, where a single sperm is injected into each egg.
After fertilization, the resulting embryos are monitored for growth and development for up to five days. The healthiest and most viable embryos are then selected for transfer into the uterus, usually two or three at a time. Any remaining embryos can be frozen for future use. Two weeks after the embryo transfer, a pregnancy test is performed to determine if the procedure was successful.
In Vitro Fertilization: A Breakthrough in Assisted Reproductive Technology
Success Rates of IVF
The success rates of IVF vary depending on several factors, such as the age and health of the woman, the cause of infertility, and the quality of the embryos. On average, the success rates for IVF range from 30-35% for women under 35 years old, and gradually decrease with age. However, advancements in technology, such as PGT and other techniques, have significantly improved the success rates, making IVF a highly effective option for couples and individuals struggling with infertility.
Ethical Concerns
While IVF has brought joy to many families around the world, it has also raised ethical concerns and controversies. One of the main concerns is the creation and storage of excess embryos, which raises questions about the status and rights of these embryos. Another concern is the potential physical and emotional risks associated with IVF, such as ovarian hyperstimulation syndrome and multiple pregnancies. Additionally, there are concerns about the commercialization of IVF and the high costs associated with the procedure, which may limit its accessibility to certain populations.
Impact on Society and Future of Reproductive Technology
The impact of IVF on society has been significant, as it has provided a solution for couples and individuals struggling with infertility and has allowed them to experience the joy of parenthood. It has also challenged traditional notions of family and parenthood, as IVF allows for alternative family structures, such as same-sex couples and single parents, to have genetically related children.
In the future, IVF technology is expected to continue to evolve and improve, with the potential to address more complex forms of infertility. There is also ongoing research into the development of artificial wombs, which could provide a solution for women with medical conditions that prevent them from carrying a pregnancy. However, this technology also raises ethical concerns and will require careful consideration before it can be used in clinical practice.
In summary, IVF has been a groundbreaking technology that has helped millions of couples and individuals achieve their dream of having a child. With continuous advancements and improvements, it has become a highly successful and widely used method for assisted reproduction. However, it also raises ethical concerns and challenges traditional notions of family and parenthood. As we continue to explore and push the boundaries of reproductive technology, it is essential to consider the ethical implications and ensure that it is used responsibly, with the well-being of all parties involved in mind.