 Can you do self-insemination at home ?
Can you do self-insemination at home ?
I anticipated that my doctor would provide more guidance.
As a journalist who has dedicated the past year to covering the U.S. government’s pandemic response, I’ve learned just how much I still have to discover. So, as an expectant mother, I felt it was wise to heed the advice from the Centers for Disease Control and Prevention (CDC) and consult my doctor regarding the COVID-19 vaccine.
His response: “It’s a personal choice.”
While I understood his perspective, it wasn’t particularly helpful. For most Americans contemplating the COVID-19 vaccine, the consensus among medical and scientific experts is a resounding “Yes!” We have robust scientific evidence affirming the vaccines’ safety and effectiveness. However, for pregnant women, the guidance is often less straightforward.
This ambiguity arises, in part, because initial clinical trials for the COVID-19 vaccines excluded pregnant and breastfeeding individuals, following a long-standing precedent in medical research. There are valid reasons for this caution: pregnancy introduces complex physiological factors, and the health of both the mother and fetus must be carefully assessed. Historical incidents, such as the thalidomide tragedy, have influenced this approach. Regulatory bodies learned from past mistakes, ensuring pregnant women are treated with extra caution.
In January, the World Health Organization (WHO) initially advised against COVID-19 vaccination for pregnant women, contradicting the CDC’s recommendation for personal choice. Fortunately, the WHO later revised its guidance to align more closely with the CDC.
Navigating this decision can be daunting for expectant mothers. How does one make a significant health choice without definitive clinical trial evidence or clear expert recommendations? While I’m not a medical professional, my role as a journalist allows me to explore information widely and engage with experts directly. Here’s how I reached my decision.
Establishing a Framework for Decision-Making
First, I established a framework for decision-making. Flipping a coin was an option, but with my health and my baby’s at stake, it made sense to assess the risks and benefits involved. This is a common practice in medicine: doctors often evaluate the potential complications of a procedure against the risks of not undergoing it.
Dr. Sarah Thompson, a specialist in Obstetrics and Gynecology at a leading university, emphasized the thorough evaluation process that regulators undertook to assess vaccine safety. After extensive clinical trials involving tens of thousands of participants, including a limited number of pregnant individuals, independent experts scrutinized the safety data for both the Food and Drug Administration (FDA) and the CDC. Organizations like the American College of Obstetricians and Gynecologists (ACOG) subsequently recommended that vaccines be made available to pregnant women. “It’s a comprehensive process, continuously reviewed by independent scientists,” Dr. Thompson explained. “This isn’t a hasty decision; the data have been meticulously vetted and are consistently monitored.”
Examining the Evidence
Next, I examined the evidence surrounding potential vaccine risks. While clinical trial data specifically for pregnant women are limited, prior studies on pregnant animals indicated that the vaccines did not pose harm. Real-world evidence is also encouraging: nearly 78,000 pregnant individuals in the U.S. reported receiving the vaccine, with no adverse effects documented for mothers or babies. Dr. Emily Harris, an obstetrician at a prominent research institution, noted, “This is quite convincing evidence that the vaccine is safe.” The CDC’s analysis of initial data revealed that vaccinated pregnant women experienced typical vaccine side effects and had no higher rates of birth complications compared to those who were unvaccinated.
Moreover, scientists have not found any clear biological reasons why the mRNA vaccines (Pfizer and Moderna) or the Johnson & Johnson vaccine would negatively impact pregnancy. The technology behind the Johnson & Johnson vaccine has been successfully used in the Ebola vaccine, which is safe for pregnant women. Other vaccines, like the flu shot, have been administered to pregnant individuals for years without incident. Unlike vaccines that use live viruses, the COVID-19 vaccines do not contain live components but instead trigger the body to produce proteins that activate the immune system to create antibodies.
Given the positive signs, experts believe that the current recommendations from organizations like the CDC and ACOG are overly cautious. Additional studies on vaccinated pregnant women are expected to be published soon. “We anticipate that forthcoming data will enhance our comfort in recommending the vaccine, similar to how we advise the flu and TDAP vaccines during pregnancy,” Dr. Thompson stated.
Contemplating the Risks of Not Being Vaccinated
I also contemplated the risks associated with not being vaccinated. Various studies indicate that pregnant individuals who contract COVID-19 face a higher risk of severe illness, potential hospitalization, or even the need for ventilation. Infection could also elevate the likelihood of preterm birth, leading to health issues for my child. With over 60 million Americans fully vaccinated, including a significant portion of the nation’s vulnerable populations, the highly transmissible variants of the virus continue to spread. “Infection rates remain high,” Dr. Thompson cautioned. “You don’t want to be the last person caught in the crossfire of a war. You want to avoid getting infected as we approach the end of this pandemic.”
I weighed the potential benefits on both sides of the vaccine debate. The main advantage of forgoing the vaccine was avoiding any rare, unforeseen complications. In contrast, the benefits of vaccination were more tangible: protection against severe COVID-19 illness, the possibility of passing antibodies to my child (as shown in several recent studies), contributing to community herd immunity, and participating in the full reopening of society with a significantly reduced risk of unknowingly transmitting the virus to at-risk individuals.
I considered my unique situation. While I could have chosen to quarantine to evade both the vaccine’s unknowns and the risk of severe COVID-19, I knew that wasn’t a feasible option for my family. Isolating myself would negatively impact my mental and spiritual well-being. After a year of virtual gatherings, I was eager to attend my sister’s college graduation and my cousin’s wedding.
My Decision
Ultimately, I decided to get the COVID-19 vaccine. I concluded that the evident benefits of vaccination far outweighed the unknown and possibly nonexistent risks. The well-documented dangers of contracting COVID-19 during pregnancy, or unknowingly spreading it to others, surpassed the advantages of a “wait-and-see” approach.
I received my first dose of the Pfizer vaccine on Tuesday and enrolled in the CDC’s v-safe post-vaccination tracker to assist researchers in understanding how the vaccine affects pregnancy and childbirth. I hope that the data collected from this tracker, along with future studies, will enable healthcare providers to offer more informed advice to pregnant patients.
This article originally appeared on a nonprofit investigative news platform based in Washington, D.C.
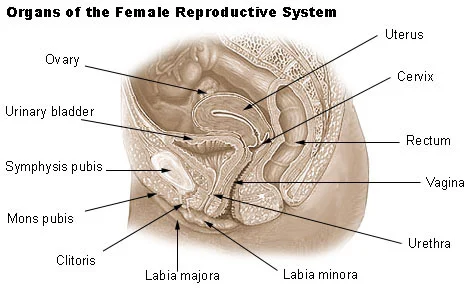
For more insights, check out this related blog post, and for further information on pregnancy, visit Intracervical Insemination, an authoritative source on the topic. Also, consider exploring this excellent resource for pregnancy and home insemination.