July 16, 2021
While waiting in my car for my COVID-19 vaccine, I offered a quiet prayer filled with gratitude, but also some unease. At five weeks pregnant, the available information on the risks and benefits of vaccination during pregnancy was limited. Nevertheless, my partner and I firmly believed that getting the COVID-19 vaccine was the right decision.
Now, after receiving both doses, I am grateful to report that both my baby and I are in good health. Preliminary studies indicate that there are no significant safety issues associated with the vaccine during pregnancy, and with the emergence of the Delta variant, I feel lucky to have this additional protection.
However, as I take a moment to appreciate this safeguard against a serious illness, another pressing health concern has emerged this summer: excessive heat. As I plan my daily walks for the coolest times, I notice that the windows of safe outdoor activity are becoming shorter and occurring earlier in the day. This trend is not surprising given that the last decade was the hottest on record, and scientists predict an increase in dangerous heat days in the coming years.
Some people may attribute these drastic temperature changes to natural cycles, but global scientific consensus points to human-induced greenhouse gas emissions as a primary cause of rising temperatures. The level of greenhouse gases like carbon dioxide has resulted in the Earth absorbing twice as much heat in the atmosphere compared to fifteen years ago. This energy imbalance contributes to higher temperatures, severe droughts, and extreme heat.
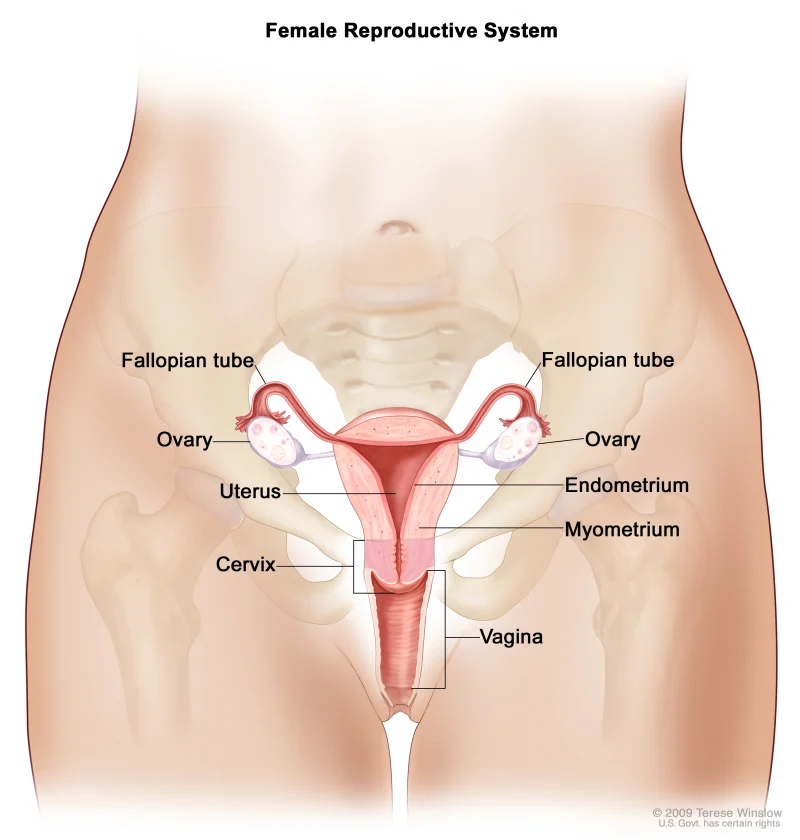
For expectant mothers like me, severe heat waves can pose significant health risks. Pregnancy already elevates the body’s baseline temperature, and when a pregnant person’s temperature reaches 102.2 degrees, the risk of heat stroke, heat exhaustion, and dehydration increases. Heat-related dehydration can reduce blood flow to the placenta, which may deprive the fetus of essential nutrients and even lead to premature labor due to decreased blood flow to the uterus.
A recent study has shown a link between high outdoor temperatures and an increased risk of premature birth by up to 21 percent. Moreover, for every degree Celsius rise in temperature during the week before delivery from May to September, the likelihood of stillbirth increases by 6 percent. Extreme heat is also associated with low birth weight and congenital heart defects.
Regrettably, the adverse effects of extreme heat disproportionately affect communities of color. Black expectant mothers are already at a higher risk for preterm birth and low birth weight, with their chances of stillbirth being double that of white mothers. Exposure to elevated temperatures exacerbates these risks. Various systemic issues contribute to these disparities. Communities of color are often situated in urban heat islands, areas that are markedly warmer than surrounding regions. These neighborhoods typically have limited tree cover and an abundance of concrete, and many residents cannot afford the increased electricity costs associated with air conditioning.
To safeguard pregnant individuals and their babies, immediate and equitable action to address climate change is essential. Creating green spaces is one strategy to mitigate extreme heat, but urban planning must prioritize the needs of marginalized communities. Energy-efficiency initiatives designed to lower utility costs must consider the structural barriers faced by vulnerable residents. President Biden’s Bipartisan Infrastructure Framework, which invests in clean transportation and power, alongside legislation like the Protecting Moms and Babies Against Climate Change Act, specifically targets the environmental health disparities linked to maternal mortality.
For me, the excitement of welcoming a child into this world is mixed with concern about ensuring their health and well-being. As I strive to do everything I can, I remain mindful of how health threats like extreme heat could hinder these efforts. My hope is that through meaningful climate action, we can create a safer, healthier world for all our children.
If you’re interested in learning more about home insemination, check out our other blog posts here. Additionally, for expert insights on this topic, visit Intracervical Insemination. For valuable information on pregnancy and home insemination, take a look at this excellent resource from Johns Hopkins Medicine.
Here are some related search queries you might find helpful:
- What are the risks of extreme heat during pregnancy?
- How to stay cool while pregnant in summer?
- Impact of climate change on maternal health
- Safe outdoor activities for pregnant women in hot weather
- Home insemination tips for aspiring parents
In summary, as a pregnant physician, I am deeply concerned about the effects of extreme heat on maternal and fetal health. The increasing temperatures pose significant risks, especially for vulnerable communities. Urgent action is needed to address climate change and protect the health of expectant mothers and their babies.