Pregnancy is often seen as a journey guided by vast knowledge and medical advancements, yet many who have experienced it know that it can still be unpredictable. Even with meticulous planning and adherence to expert advice, there are many factors in pregnancy that remain elusive. This uncertainty can be even more daunting when complications arise, such as placenta accreta. If you or someone you know has received this diagnosis, it’s crucial to understand its symptoms, risks, treatment options, and management strategies.
What is Placenta Accreta?
Placenta accreta occurs when the placenta attaches itself too deeply into the uterine wall. According to health experts, this condition can lead to serious complications, including the placenta not being delivered naturally after childbirth and potential heavy bleeding when attempting to remove it. Generally, there are no noticeable symptoms during pregnancy, although some may experience vaginal bleeding in the third trimester.
Causes of Placenta Accreta
While researchers have yet to identify a definitive cause for placenta accreta, various risk factors have been identified. Many individuals with this condition have abnormalities in the uterine lining, often due to scarring from a previous C-section or other uterine surgeries. Other contributing factors include:
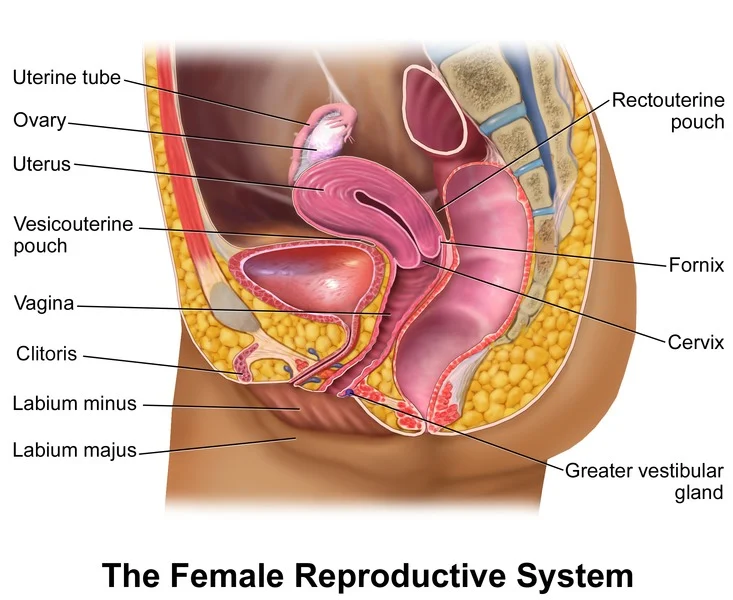
- Placenta Position: If the placenta is low or partially covers the cervix (placenta previa), the risk of placenta accreta increases.
- Maternal Age: Women over 35 are at a higher risk.
- Previous Pregnancies: The likelihood increases with each subsequent pregnancy.
Types of Placenta Accreta
There are two additional forms of placenta accreta based on how deeply the placenta penetrates the uterus:
- Placenta Increta: The placenta invades the uterine wall but doesn’t pass through it.
- Placenta Percreta: The most severe form, where the placenta penetrates through the uterine wall and can affect surrounding organs.
Diagnosis of Placenta Accreta
Placenta accreta may be detected during routine ultrasounds, but it is often diagnosed at delivery. If suspected during pregnancy, ultrasounds are the primary diagnostic tool, although an MRI may be utilized in certain cases. It’s important to note that not all cases are identified before delivery, but this often does not affect the outcome.
Treatment Options
Treatment strategies for placenta accreta depend on the timing of diagnosis and severity. Surgical intervention is frequently necessary, which may involve the complete or partial removal of the placenta. Techniques vary from cord traction, which is less invasive, to manual removal, where the doctor physically extracts the placenta. In more severe cases diagnosed early in pregnancy, a C-section followed by a hysterectomy may be planned to prevent excessive blood loss during delivery.
Risks of Retained Placenta
Immediate removal of the placenta is essential after childbirth. If it remains in the uterus, it can cause hemorrhaging and other serious complications. The placenta should ideally be delivered within 30 minutes post-birth to avoid risks like uterine scarring and the need for a blood transfusion or hysterectomy, which can be life-threatening without prompt treatment.
For further information on this topic, you can check out one of our other blog posts here. If you’re looking for more resources, this site provides valuable insights and expert advice. For comprehensive information on pregnancy, visit Medical News Today.
Related Search Queries:
- What is placenta accreta?
- Symptoms of placenta accreta
- How is placenta accreta treated?
- Risks of retained placenta
- Diagnosis of placenta accreta